
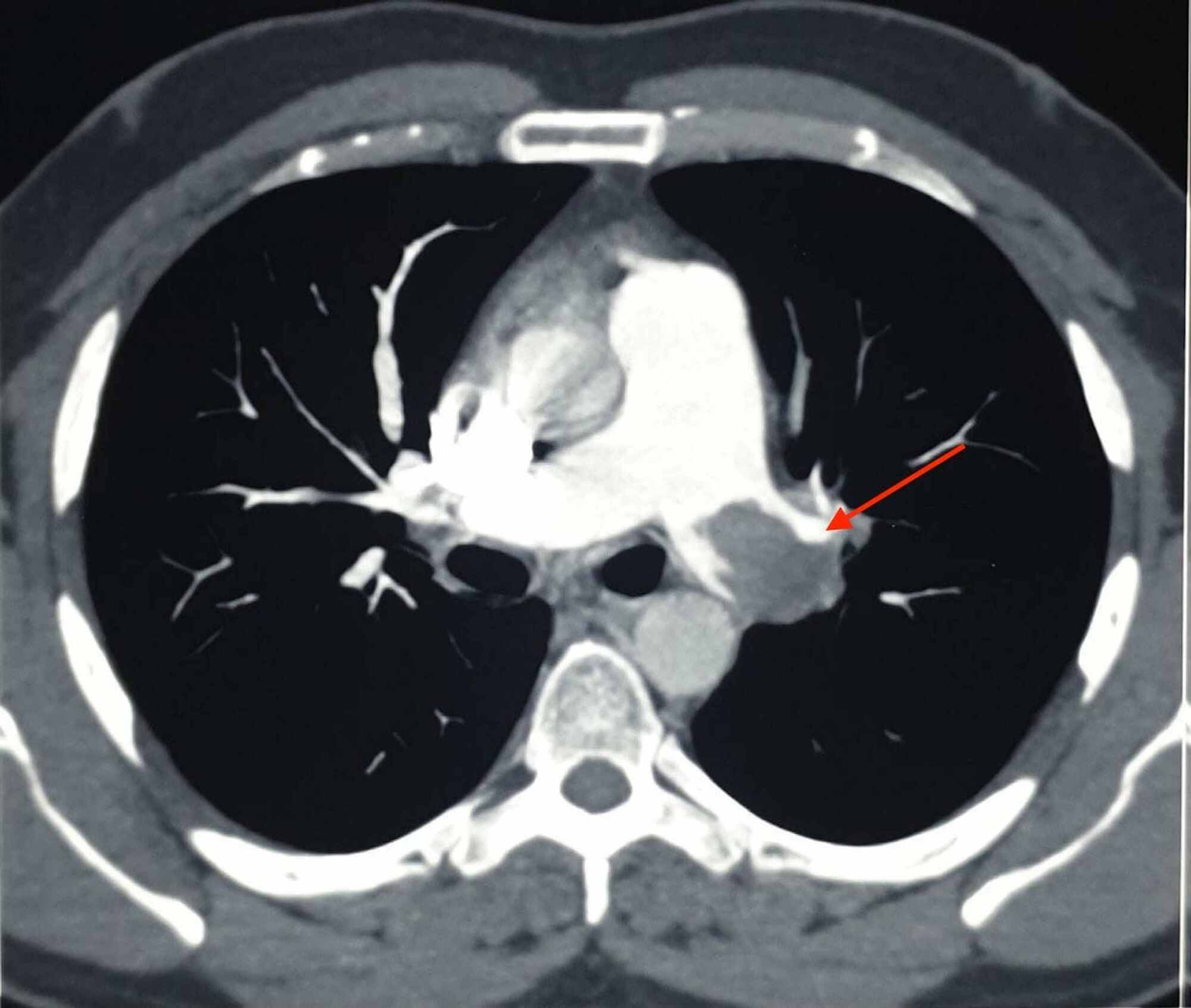
The patient was thought to have a high-risk DVT due to its extension, so the plan was to treat him with parenteral anticoagulation for 5 to 7 days and then switch to direct oral anticoagulation (DOAC). No incidental PE was seen in the CT chest ( Figure 1). With his history of RCC, the patient had a computed tomography (CT) of the chest and abdomen/pelvis with IV contrast to rule out any masses/cancers as an underlying possible provoked cause of his acute DVT, but all came back negative.
#Massive pulmonary embolism full#
The patient was admitted to the telemetry floor after he was started on a heparin drip with a bolus for full anticoagulation. The patient was given analgesics orally, but his pain did not subside so he was started on intravenous (IV) analgesics. His LE venous Doppler showed acute DVT from the proximal right superficial femoral vein through the popliteal vein and involving the calf veins. His basic laboratory workup including complete blood count, prothrombin time, partial thromboplastin time (PTT), international normalized ratio (INR), and the comprehensive metabolic panel was normal ( Table 1). The rest of the physical examination was unremarkable. No cyanosis or blanching of the lower extremities. Dorsalis pedis and posterior tibial arteries pulses were +3 bilaterally.

His physical examination showed swelling of the right LE with erythema, edema, tenderness, and positive Homans’ sign. He was not compliant with his medications that included Lisinopril and atorvastatin.
No history of recent travel, trauma, immobilization, or surgery. A 46-year-old Caucasian male with a history of hypertension, obesity, hyperlipidemia, and left renal cell adenocarcinoma (RCC) a few years ago status post partial nephrectomy and was in remission, presented to the emergency room (ER) with a 10-day history of severe right lower extremity (LE) pain, redness, and swelling.


 0 kommentar(er)
0 kommentar(er)
